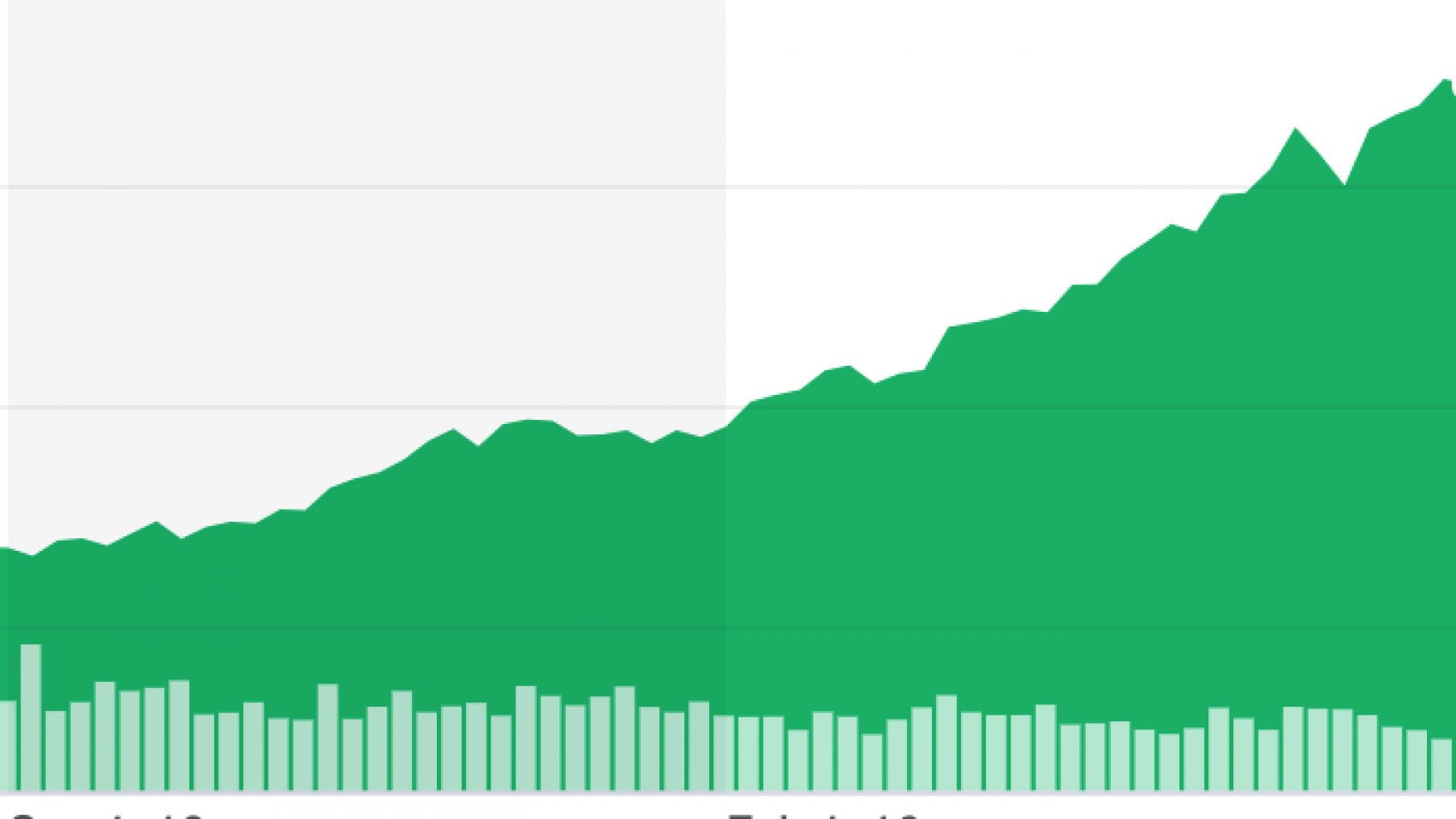
It’s July and that means earnings season. We get a view of the workings of UnitedHealth Group (“UHC”), the “diversified health care company dedicated to helping people live healthier lives and helping make the health system work better for everyone.” We’ve all carried a United Healthcare card at one point. UHC is the largest healthcare company in the US and has a long list of impressive stats: over $200B in revenue, 27M people enrolled in commercial plans, close to 10M Medicare Advantage and Medicare Supplement seniors, 92M people through Optum, 4.8M health savings accounts, and owner of hundreds of surgery centers. It generates north of $11B in free cash flow per year and its stock has trounced the S&P 500 and its peer group over the last 5 years: a 30% compounded annual return vs. <11% for the S&P and 23% for its peer group.
Since analysts want to be right with all their short-term modeling and projections (on a side note, I recommend a book called The Number: How the Drive for Quarterly Earnings Corrupted Wall Street and Corporate America) and management wants to exceed the expectations they set, analysts’ questions and company metrics are often about what moves stock prices but peppered with some large standalone numbers that require some sleuthing.
Of the many things discussed, it’s worth highlighting three things that I learned from UHC’s July 15th earnings call:
1) Medical and prescription drug trends:
For all the talk of high Net Promoter Scores, AI, machine learning, analytics, industry heft, and surgery center savings on hip replacements, UHC’s commercial medical trend is forecast at 6% (+/- .5%), or 2-3x inflation. They break this out as 4% from price increases and 2% higher utilization; OptumRx filled 3% more prescriptions quarter-over-quarter. So while the bigger increase is cost inflation, utilization is also moving up. Healthcare’s share of the GDP pie continues to bulge. That’s bad for the US in aggregate, but growth above inflation bodes well for investors, and other select groups.
2) Big numbers, but hold on:
Rally is their digital front door and through it $1 billion in incentives have been paid. “Consumers earned these incentives for taking real actions to improve their health, like receiving biometric screenings.” The problem with biometric screenings is they cost money to administer, and you have to pay people incentives to get them (something a deep dive into the Kaiser Family Foundation Employer Survey data proves), they often flout the United States Preventive Services Task Force recommendations on screening frequencies, and they create false positives and extra tests, especially problematic for healthy people but great for UHC. More healthcare dollars is good for business.
“This year our customer advocates will help people, in real time, schedule hundreds of thousands of doctors’ appointments to close specific gaps in care. Together, these services are helping client’s advance quality, lower costs and improve consumer satisfaction. This integrated approach improves pharmacy adherence by 12%, while helping reduce hospital admissions and ER use by 6%.” I ran the numbers on the hospital and ER savings, and it amounts to <$2 per person per month.
“In our Medicare products, value-based care is driving…a 3% increase in the number of seniors with regular doctor visits.” Yawn.
3. Whose risk?
The “Cadillac tax” won’t go away and is hotly debated. This is the tax of 40% beyond a base benchmark dollar value of $10,200 for a single employee and is meant for plans that are overly generous–it has been pushed back to 2022. Economists, and other reasonable people, believe healthcare benefits beyond a certain level should be treated as compensation. As it now stands, given the cost and health plan structures, only around 5% of people would trigger the tax. However, that would change over time since the tax is indexed to inflation and healthcare is stubbornly growing faster than that. UHC refers to it as a headwind and says “the return of the health insurance tax in 2022 will cause higher premiums and lower coverage levels for people, and we will be advocating on behalf of our customers and consumers for a delay or outright repeal of this tax.” They don’t like it since lower plan values and higher cost sharing needed to avoid the tax means less revenue for UHC. Healthcare policy makers, comfortable in their Ivory Towers, actually designed the tax to incentivize employers to seek greater sources of value of care through contracting, etc. (not realizing that hospitals have 2-4% profit margins and not much room to budge); they chose the easier path of increasing cost share to employees.
Higher premiums = higher revenues = higher profits = juicier equity returns. This reminds me of how a large broker lists as a top risk: “Our ability to generate premium-based commission revenue may also be challenged by the growing desire of some clients to compensate brokers based upon flat fees rather than variable commission rates. This could negatively impact us because fees are generally not indexed for inflation and do not automatically increase with premiums as commissions do.” What’s best for the insurer is not always best for you and me.
UHC is working exactly as intended, and in many ways is doing great things with all it delivers. After all, they are not responsible for our nation’s poor collective health, but higher costs and programs that deliver more value to shareholders are at the front. Corporate platitudes aside, the companies buying the insurance have power since they control budgets. They just need to ask better questions, be more informed, and realize what doesn’t work, even if the results are modest. Innovation in healthcare tends to be inflationary. A new recipe is needed to keep costs and utilization down.